Introduction
Veins are an essential part of the circulatory system, responsible for transporting deoxygenated blood back to the heart. While veins are often overlooked in discussions about health, they play a vital role in maintaining proper circulation and overall bodily function. When veins become damaged or impaired, however, a range of medical conditions can arise, including varicose veins, spider veins, deep vein thrombosis (DVT), and venous insufficiency. These conditions not only affect physical health but can also impact a person’s appearance, mobility, and quality of life.
This article will delve into the anatomy and function of veins, common vein-related health concerns, and the various treatments available for managing or correcting these conditions. By understanding the underlying causes of venous issues and the treatments that are available, individuals can make informed decisions about their vascular health.
Part 1: The Anatomy and Function of Veins
1.1 The Circulatory System: An Overview
The circulatory system, consisting of the heart, arteries, veins, and capillaries, is responsible for delivering oxygen and nutrients to the body while removing waste products like carbon dioxide. The system is divided into two main parts:
- The Systemic Circulation: This part of the circulatory system carries oxygenated blood from the heart to the body through the arteries and returns deoxygenated blood back to the heart through the veins.
- The Pulmonary Circulation: This part involves the transport of deoxygenated blood from the heart to the lungs for oxygenation and back to the heart.
Veins specifically are responsible for transporting deoxygenated blood from the organs and tissues back to the heart. They play a crucial role in maintaining blood pressure and blood flow throughout the body.
1.2 Structure of Veins
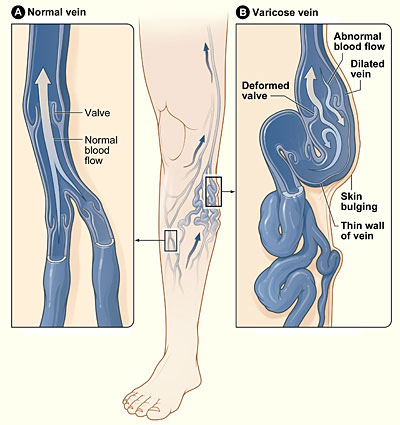
Veins differ in structure from arteries. They are generally thinner, have less muscular and elastic tissue, and feature one-way valves that prevent blood from flowing backward. These valves are particularly important in preventing the backflow of blood in the lower extremities, where gravity works against the natural flow of blood back to the heart.
- Vein Wall Layers: Like arteries, veins have three layers:
- The Tunica Intima: The innermost layer, consisting of endothelial cells that provide a smooth surface for blood flow.
- The Tunica Media: The middle layer, composed of smooth muscle and elastic tissue, helps the veins contract and regulate blood flow.
- The Tunica Externa: The outermost layer, made of connective tissue, provides structural support to the vein.
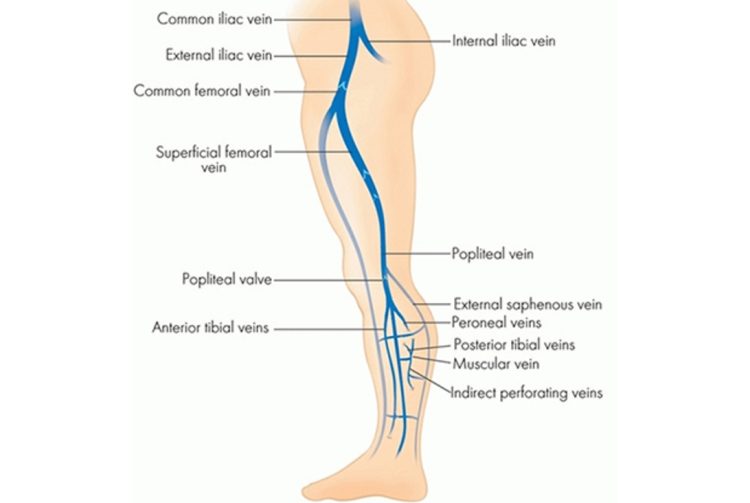
1.3 Types of Veins
- Superficial Veins: These veins are located just beneath the skin and are responsible for returning blood from the outer parts of the body to the heart.
- Deep Veins: Found deeper within the body, these veins carry blood from the organs and muscles. The deep veins are typically larger and more muscular than the superficial veins.
- Perforating Veins: These veins connect the superficial veins to the deep veins. They are crucial for maintaining proper venous circulation.
Part 2: Common Vein-Related Health Concerns
2.1 Varicose Veins
Varicose veins are enlarged, twisted veins that typically appear on the legs. They occur when the valves inside the veins weaken, causing blood to pool and the veins to stretch. As a result, the veins become visible under the skin and can cause discomfort, swelling, and aching.
- Causes of Varicose Veins: The primary cause of varicose veins is increased pressure in the veins, which can occur due to factors such as:
- Genetics: Family history can play a significant role in the development of varicose veins.
- Aging: As we age, the valves in our veins can weaken, making it harder for blood to flow effectively.
- Pregnancy: Hormonal changes and the increased pressure on the veins during pregnancy can lead to varicose veins.
- Obesity: Excess weight puts additional pressure on the veins in the lower extremities, leading to the development of varicose veins.
- Prolonged Standing: Occupations or activities that involve standing for long periods can increase pressure in the leg veins.
- Symptoms: The most common symptoms of varicose veins include:
- Visible, bulging veins, typically blue or purple in color.
- Aching or heavy feeling in the legs.
- Swelling or tenderness in the legs or feet.
- Skin changes near the affected veins, such as discoloration or ulcers.
2.2 Spider Veins
Spider veins are smaller, thinner blood vessels that appear near the surface of the skin. These veins are often red or blue and resemble spider webs or tree branches. They are generally not as serious as varicose veins but can be a cosmetic concern for many people.
- Causes of Spider Veins: Like varicose veins, spider veins are often caused by:
- Genetics
- Hormonal changes (e.g., pregnancy, menopause, birth control use)
- Sun exposure (which can damage the skin and blood vessels)
- Age and prolonged standing
2.3 Deep Vein Thrombosis (DVT)
Deep vein thrombosis is a serious condition that occurs when a blood clot forms in a deep vein, usually in the legs. DVT can be dangerous because the clot can break loose and travel to the lungs, causing a pulmonary embolism.
- Symptoms: The symptoms of DVT can vary but may include:
- Swelling or redness in one leg.
- Pain or tenderness in the affected area, especially when standing or walking.
- Warmth in the skin over the clot.
- Risk Factors: Some common risk factors for DVT include:
- Prolonged immobility (e.g., sitting for long periods during travel or hospitalization)
- Surgery or injury to the veins
- Obesity
- Pregnancy
- Smoking
- Certain medical conditions, such as cancer or heart disease
2.4 Chronic Venous Insufficiency (CVI)
Chronic venous insufficiency occurs when the veins in the legs cannot pump enough blood back to the heart. This condition can lead to swelling, pain, and skin changes in the lower legs and feet.
- Symptoms: Common symptoms of CVI include:
- Swelling in the lower legs or ankles.
- Pain or cramping in the legs, particularly after standing or sitting for long periods.
- Skin changes, such as darkening or ulceration.
- Varicose veins.
- Causes: CVI is often caused by damage to the veins’ valves, which leads to poor blood flow and pooling of blood in the legs. This can occur due to factors such as:
- Previous DVT or other venous problems.
- Obesity.
- Prolonged standing or sitting.
2.5 Venous Ulcers
Venous ulcers are open sores that develop on the skin, typically near the ankles or lower legs. These ulcers are often a complication of chronic venous insufficiency and occur when blood flow to the skin is inadequate.
- Symptoms: Venous ulcers can cause:
- A painful, open wound that is difficult to heal.
- Swelling in the affected area.
- Discoloration of the skin surrounding the ulcer.
Part 3: Treatment Options for Vein Conditions
3.1 Conservative Treatment and Lifestyle Changes
For some individuals, making lifestyle changes and taking conservative steps can help alleviate the symptoms of vein-related conditions.
- Compression Stockings: Compression stockings help to improve circulation by applying pressure to the legs. They are particularly effective for conditions like varicose veins, spider veins, and chronic venous insufficiency.
- Exercise: Regular physical activity, especially walking and leg exercises, can help improve circulation and prevent blood from pooling in the veins.
- Weight Management: Maintaining a healthy weight can reduce the pressure on the veins, particularly in the legs.
- Elevating the Legs: Elevating the legs above the level of the heart can help reduce swelling and improve venous return.
3.2 Medical and Surgical Treatments
If lifestyle changes do not provide sufficient relief, medical procedures may be necessary to treat vein conditions.
- Sclerotherapy: Sclerotherapy is a common treatment for spider veins and smaller varicose veins. It involves injecting a solution into the affected vein that causes the vein to collapse and be absorbed by the body.
- Laser Therapy: Laser treatments use focused light to treat varicose veins and spider veins. The heat from the laser causes the vein to close and eventually disappear.
- Endovenous Laser Treatment (EVLT): EVLT is a minimally invasive procedure used to treat larger varicose veins. A laser fiber is inserted into the vein, where it uses heat to collapse and seal the vein shut.
- Vein Stripping and Ligation: In more severe cases of varicose veins, vein stripping and ligation may be performed. This involves removing
or tying off the affected vein.
- Ambulatory Phlebectomy: This procedure is used to remove varicose veins near the surface of the skin. It is minimally invasive and performed under local anesthesia.
3.3 Treatment for Deep Vein Thrombosis (DVT)
- Blood Thinners (Anticoagulants): The primary treatment for DVT is anticoagulant medication, which helps prevent the clot from growing and reduces the risk of the clot breaking off and traveling to the lungs.
- Thrombolytics: In some cases, clot-dissolving medications may be used to treat more severe DVT.
- Compression Stockings: These can help prevent complications and reduce swelling in the affected leg.
3.4 Preventive Measures
Preventing vein conditions, particularly DVT and chronic venous insufficiency, is essential for maintaining vascular health.
- Regular Movement: If you sit for long periods, especially during travel, try to get up and move around every 1-2 hours to promote blood flow.
- Stay Hydrated: Proper hydration helps maintain healthy blood viscosity.
- Avoid Smoking: Smoking can damage the walls of blood vessels and increase the risk of vein disease.
- Elevate Legs: Elevating the legs regularly can reduce the pressure on the veins and prevent blood pooling.
Conclusion
Vein health is essential to overall well-being, and understanding the different types of vein conditions is the first step in managing them effectively. While conditions like varicose veins and spider veins are often considered cosmetic, they can have significant implications for a person’s physical comfort and quality of life. More serious conditions like DVT and chronic venous insufficiency require prompt medical attention to prevent complications.
Fortunately, there are numerous treatment options, ranging from lifestyle changes and conservative treatments to advanced medical procedures. By staying informed and seeking timely medical advice, individuals can maintain optimal vascular health and reduce the risk of more serious complications.